Joletta Belton (Jo) writes a blog on living with chronic pain which covers a range of topics related to her story. In this post she talks about the language clinicians use when talking to patients.
I’m writing about language…again! It’s because this year I have had the great honor to speak at a number of conferences, and it’s come up every time.
One of the most important talks I’ve ever given was at the Paincloud Convention. It was the most vulnerable I’ve ever been on stage, probably the most vulnerable I’d ever been in public period (including on these pages).
As I wrote in my last post, the month before Paincloud my friend Chris Caldwell had said that people learn more from our weaknesses than our strengths. That resonated with me, and I wanted to bring that to the stage in Oslo. My most read post, after all, prior to the one I wrote about Cognitive Functional Therapy, was on shame and resentment.
It was a post I was terrified to share, so deeply personal. So deeply human.
This stuff ain’t easy
Shame is not something that is easy to talk about. Feeling weak and unworthy are not easy things to talk about. Being resentful and angry are not easy things to talk about. But I was all those things, and for a long while.
I was ashamed, I felt weak and unworthy, I was angry and resentful.
Pain sucks. Losing so much because of pain sucks. Pain that doesn’t make sense, the life that it leads to that doesn’t make sense, is hard, difficult, scary shit to deal with.
Because that talk was so meaningful to me, I wanted to share some of the bits I feel are really important. Bits that I can’t talk about enough because they’re just so damn important.
I’ll ask here, as I asked at Paincloud, to please just listen, without forming judgments or responses. Bear witness. Be a compassionate presence, which is all you can be sometimes, and that is enough.
What you say matters
The words we hear from others, including you, become our own words. They become a part of how we make meaning of our experiences, a part of our belief system about ourselves, who we are, what we’re capable of. What we’re not capable of, who we aren’t.
Over the years of my treatment I was told many things about myself. You may argue that it was told to me about my hip, or my posture, or my pain, or my status within the worker’s compensation system, but none of those things can be separated from me as the person. From me as Jo who lived daily with that hip, those postures, that pain, and the labels assigned to me.
The words and labels that came to define me
I was told I was torn, weak, damaged, unstable, crooked, asymmetrical, out of alignment, counter-rotated, degenerating. I was diagnosed with femoracetabular impingement and a labral tear before surgery, after surgery with post-surgical persistent pain, SI joint dysfunction, discogenic bulging with radiculopathy, annular tears.
I failed conservative care. I failed physical therapy, injections, chiropractic. Then I failed surgery, and PT again. I was the failure, the treatments never failed me.
All the while my workers compensation paperwork was full of NOs. No lifting, no squatting, no crawling, no awkward positions, no sitting for longer than 15 minutes (including driving), no climbing, no running…NO NO NO NO NO.
You can’t do these things. You won’t do these things. If you do, your claim will be in jeopardy. Your character questioned, your motives suspect. You’re seen as trying to game the system rather than seen as trying to get better, to heal, to live some sort of life worth living.
The end of a career…
The biggest NO of all…no return to work as long as there is still pain.
No return to work if there was still pain.
This fed into my notions of pain being damage, intolerable, unacceptable. Bad, scary, dangerous. It’s what forced me into medical retirement, at the age of 35, from the career that had defined me. All because it was too painful to sit, because I couldn’t fake that it wasn’t, because I believed I was broken.
All because I came to believe I was all those things I was told I was. That I was weak, unstable, out of alignment, torn, damaged, degenerating, dysfunctional, crooked, twisted. That I couldn’t run, squat, lift, climb, sit.
There was a time I believed quite the opposite – this is me on the Inyo Complex Fire in 2007. After an 8 hour drive to the fire we worked the fireline for 12 hours. Lots of sitting during the drive, lots of climbing, running, squatting, lifting, pulling, hiking, and awkward positions fighting the fire all night!
A life sentence…
All these labels and NOs and failed treatments added up to whole person impairment and a disability rating. I was declared permanent and stationary, which in medico-legal terms meant I had plateaued. There was nothing more to be done. I was NEVER going to get better.
At the lowest point of my life, the most painful and hopeless, the darkest and most despairing, I was declared by the experts to be permanent and stationary.
Stuck there. Forever.
Is it a wonder we became fearful? Avoidant? Worried? Anxious? Depressed? Frustrated? Sad? Angry? Hopeless? Despondent? Withdrawn?
Is it a wonder we might become that ‘difficult patient’ when our hope has been taken from us and the blame for our pain is set squarely on our shoulders?
Language used in the clinic matters, too
During my talk at Paincloud I shared a story of one of my lowest points in seeking care. I was going to about my fifth physical therapy clinic in three years. My third since my surgery.
I was still hopeful, despite not having much success in PT and manual therapy, and even having some downright scary interactions. Like when one very nice PT showed my husband how to do a manual thrust move to put my SI joint ‘back in’. We did it once and it was painful and terrifying for both of us and we never did it again.
I was still hopeful, despite being told my spine was twisted on it’s axis (?!), that I had an extra lumbar vertebra (I don’t), that my shoulders were rotated and my pelvis counter-rotated (still are, yet have no pain now) and that was why I was in pain.
Or was it the tibial torsion from a broken leg in high school, 20 years before?
I also had too much anterior tilt…and too much posterior tilt. It all got confusing after a while, with no one really agreeing. Obviously, none of that was ‘the answer’ as I was still searching for the next ’cause’ and promised ‘fix’.
A side note on biases…
I loved physical therapy (still do!). PT supported all of my pre-pain biases. I had been a firefighter, a crossfitter, a runner. I was certified in FMS and TRX Sports Medicine and all sorts of other weekend courses that had me believing I knew everything about the human machine and how to keep it running optimally.
I lifted heavy for years and thought it could fix anything, and despite years of not getting better, I still thought fixing my posture, my asymmetries, my imbalances – that ‘correcting’ all of it – would fix my pain.
I was a beast in PT. Single leg squats – BAM! TRX triple threats – BAM! I was uber-functional and got back to being strong (can’t go wrong!) fairly quickly.
But I couldn’t sit, or engage with life, or be who I wanted to be. I was in debilitating pain every. single. day.
The labels, and the solutions, were easy for me to adopt, because they were what I’d already believed. It took me going through my own pain experience, and seeing that ‘fixing’ all of these things wasn’t the answer, that I began to question those beliefs.
But that came later. (The cognitive dissonance was strong when I learned the complexities of pain! That my body wasn’t just a broken machine that could be fixed with some body mechanics.)
This next clinician would be the answer, I was sure.
After years of failure, years of NOs, years of diminishing hope, I was still hanging on, still trying, still seeking answers. The morning before I headed to this new PT was a difficult one, as were all my mornings back then.
It took me 20 minutes just to get out of bed, doing gentle stretches before the stiffness and pain would let up enough for me to sit up and get my feet on the floor. Then to the living room to begin my daily routine of some static and dynamic stretches that lasted about an hour, just so I could face the day.
Afterward I stood at the kitchen counter to drink coffee and eat breakfast. Sitting was unbearable so I stood all day, even on my commute to work – I took the train, which took longer but at least I could stand.
I had to drive to my appointment, though. Driving was my nemesis, my most painful activity. It brought involuntary tears to my eyes every time (despite being set up with towels to sit on and lumbar and scapular rolls by a former, really kind PT). It was why I rarely left my house.
But I drove this day. I pulled into the parking lot, gathered myself, made sure my eyes were dry and clear, went in through the clinic doors…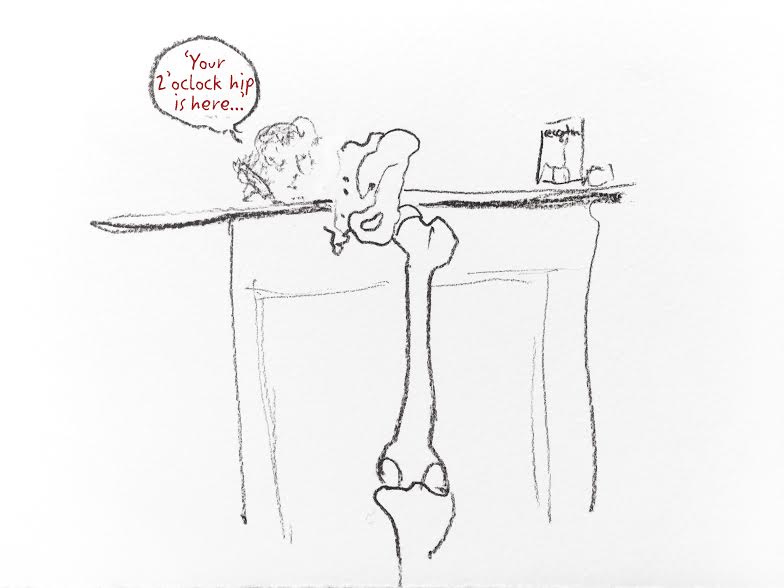
Created for me for Paincloud by Soula Mantalvanos
Dehumanized
After I signed in and was standing at the counter to fill out paperwork, the woman at the front desk told the therapist standing through the clinic door ‘your 2 o’clock hip is here’.
That’s what I was. A 2 o’clock hip. Not a human being. Not a person who had been struggling with pain for three years. Not a person who had lost their career as a firefighter, and with it lost my identity, sense of self-worth, future. Not a person who’d completely disengaged from the world I had once been so much a part of. Not a person who had stopped doing all of the things that were meaningful to me, who disconnected from all of my friends and family.
I no longer ran, no longer lifted, no longer fought fires and saved lives. No longer camped, hiked, or traveled to see family. No longer went out for drinks with friends or dinner with my husband, no longer watched movies at home, sitting on my couch, because the pain was intolerable. No longer drove, no longer played…I was no longer me.
I was just a painful hip.
I’m sure the woman was a nice person with no malicious intent. But that doesn’t change the effect of those words, or that they happen often in healthcare. That is how we are often referred to. We’re a painful back, a painful hip, a painful knee, a painful whatever. We are a diagnosis. A condition. A disease. A patient. An appointment time.
Too often, we are not seen as people first. Not seen as people who are living with pain and seeking care because we are unable to cope on our own.
Compliance, motivation, adherence…
This is why it infuriates me when I hear clinicians say their patients just aren’t motivated. That’s bullshit. When I hear that, I hear a clinician who doesn’t truly understand pain and people.
If we are still alive, we are motivated by something.
I just happened to be motivated by exercise because it was a part of my makeup before pain. Physical therapists loved me for that. I was a model patient, I did all of my homework, always, never missing a day in three years. I would do hours of friggin’ homework. Homework that supported both my and my therapists’ biases.
Despite all my ‘compliance’ and ‘motivation’, though, I was still in debilitating pain. Pain I could not make sense of. I was still forced to medically retire. I still couldn’t sit or engage with my life.
That was looked over all too often.
My pain didn’t matter. How it affected my life didn’t matter. My range of motion and adherence to home exercises was what mattered.
And that makes no sense.
Our words matter
2 o’clock hip. Weak, unstable, dysfunctional. Torn, damaged. Failure. The implied frailness and breakability.
All of these words, all of the nos, all of the labels – the boxes I was put in – became a part of what I believed about myself, what I believed I was capable of, what I believed I could and couldn’t do.
I became those labels, those words, those NOs. I became small and weak and frail as I withdrew inward, into the shell of my former self.
Challenging preconceptions
I was not some impressionable sensitive snowflake. I was strong, capable, fit. I was one of 25 female firefighters in a department of 1000 firefighters and I could hang with the boys. I was well-respected in a job that’s hard to gain respect in.
I could handle stress and pain and difficulty. I grew up in a family where you walk pain off unless there’s bone showing.
I was a problem solver, I helped people get through their worst days. Until every day became my worst day.
I swear. A lot. Still. So I’m not saying mind your language because it might be offensive or not politically correct, I was a firefighter for fucks sake. One who grew up in the Detroit area where there’s no such thing as swear words, they’re just part of our vernacular.
What I am saying is that the way we make sense of the world, of our experiences, of ourselves, is through language. The way we make meaning of our existence and share that existence with others is through words.
So language matters. A lot.
Truth
Sticks and stones may break my bones,
but words can also hurt me.
Stones and sticks break only skin,
while words are ghosts that haunt me.
Slant and curved the word-swords fall
to pierce and stick inside me.
Bats and bricks may ache through bones
but words can mortify me.
Pain from words has left its scar
on mind and heart that’s tender.
Cuts and bruises now have healed;
it’s words that I remember.
~Barrie Wade
My plea
Hold compassion in your hearts. The more difficult a patient may be, the more compassion they likely need.
Listen. Hear us. Know us.
Build us up. Tell us we are strong, adaptable, capable, resilient. Show us we are those things.
Recognize our persistence, patience, and courage.
Help us make sense of things, using our story to guide you. We’ve heard a lot of nonsense over the years, we’ve heard a lot of inaccurate and harmful things, so be patient as we try to come to new understandings.
Guide us back to our meaningful lives. We need your help to get there.
Plant seeds and help us nourish them. This stuff takes time, but there is realistic hope for all of us.
Thanks
Thank you for reading. Thank you for the good work you do. Thank you for listening. It is together that we can make meaningful change.


Stay Connected